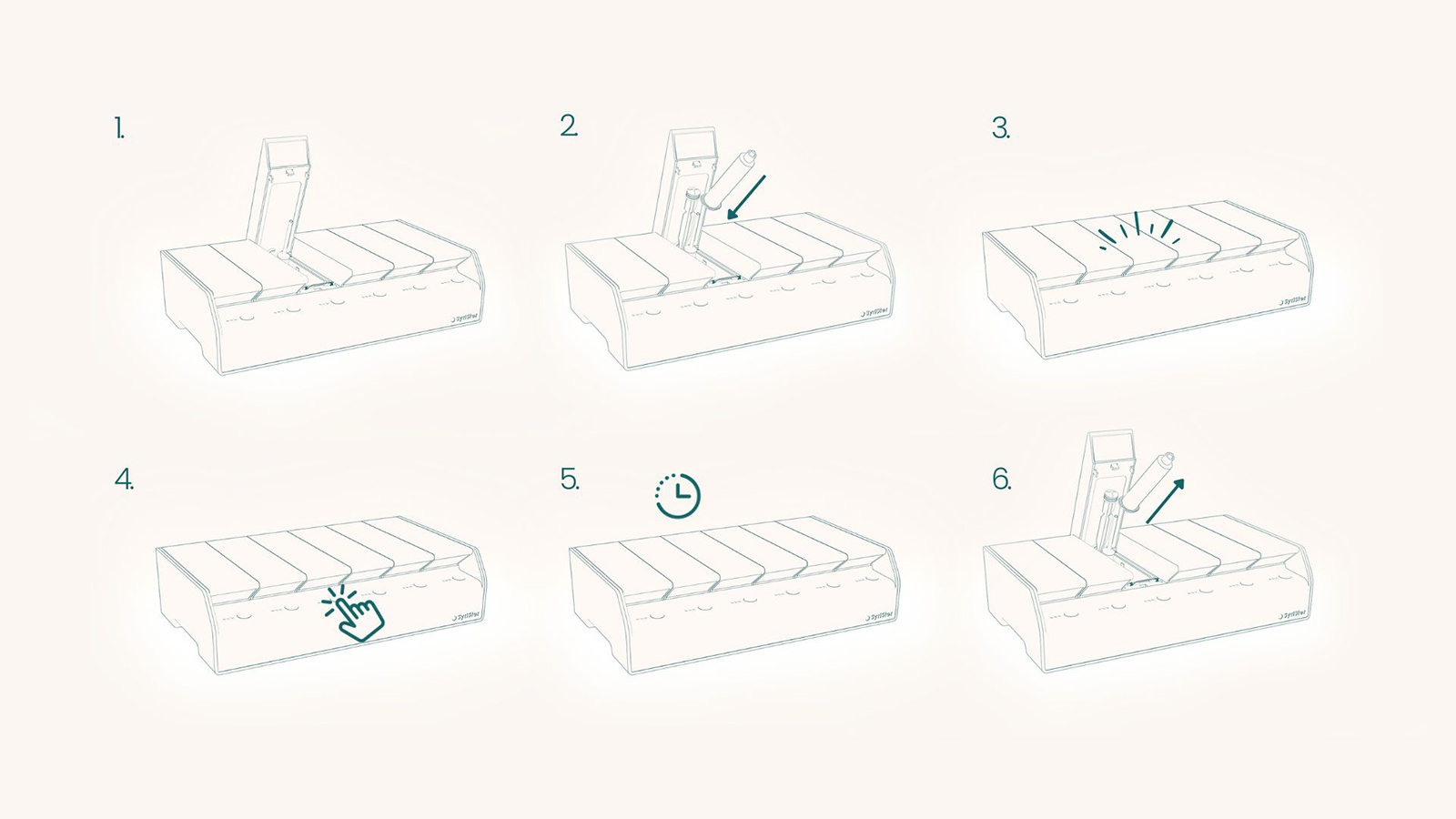
The design process began by interviewing paramedics, SES, and SAR personnel to gain insight into processes and systems that are causing inefficiencies in their jobs. These interviews identified a need for safe re-use of critical and commonly used medical supplies, particularly in crisis zones where re-use is unavoidable.
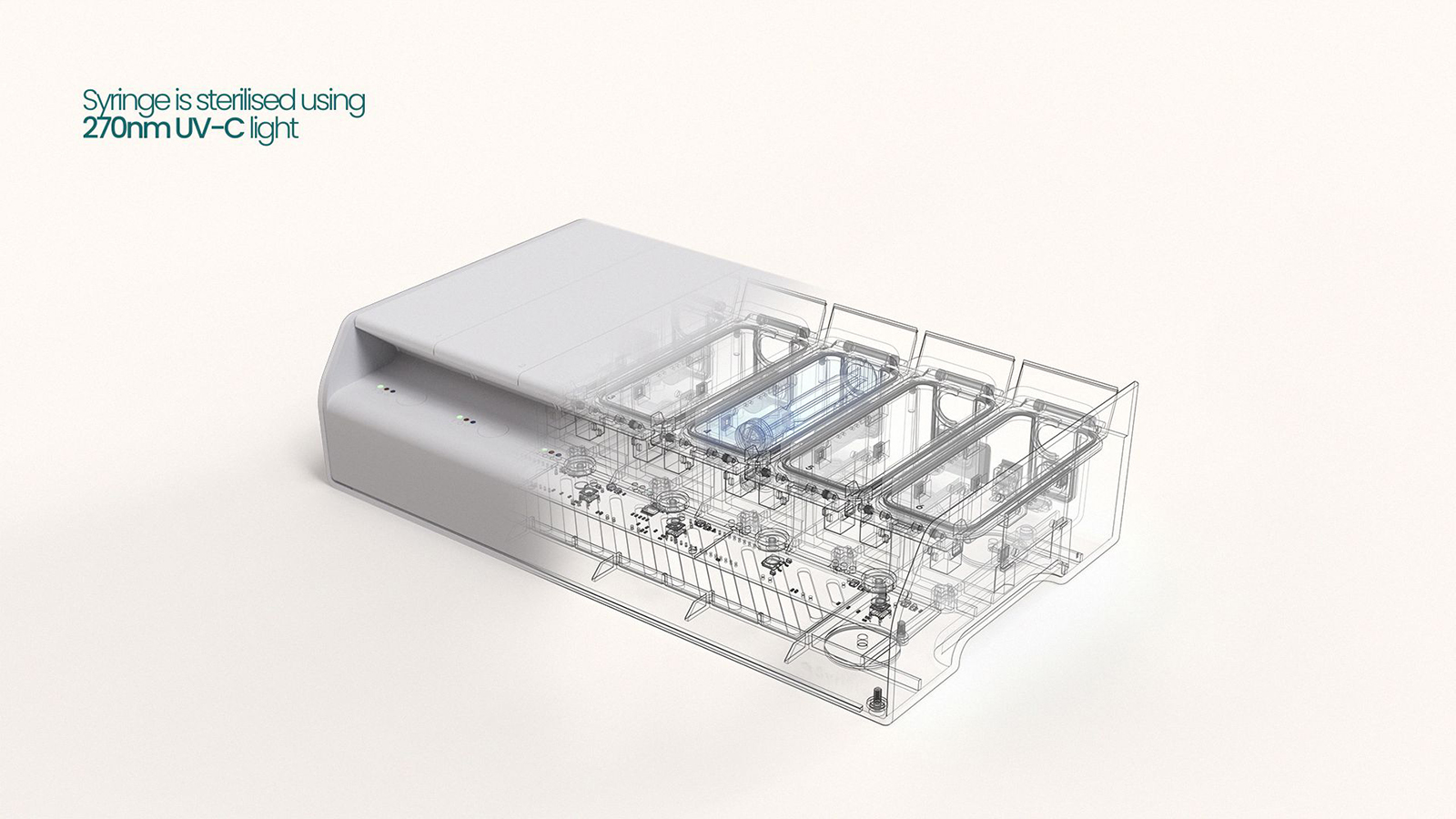
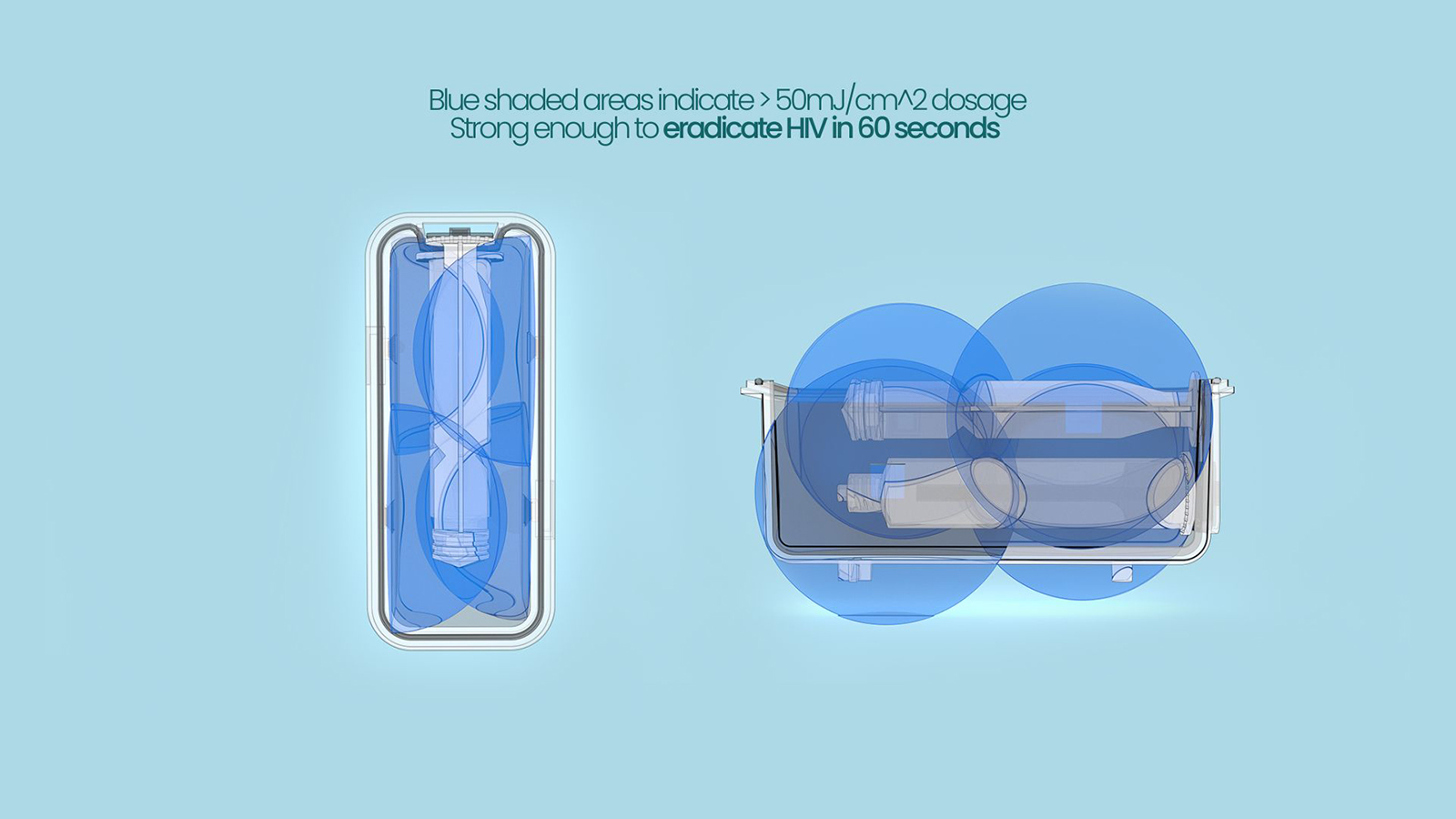
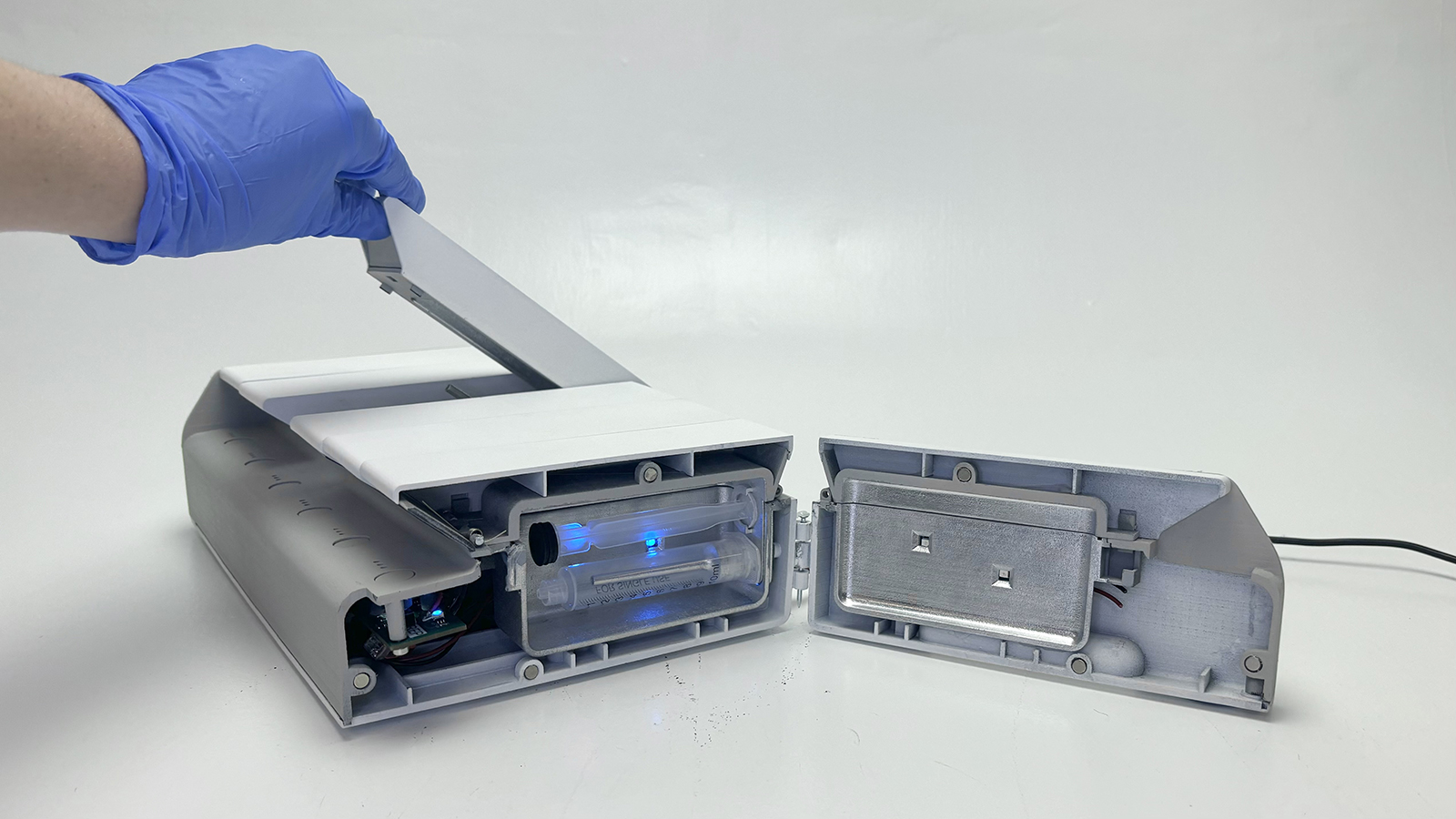
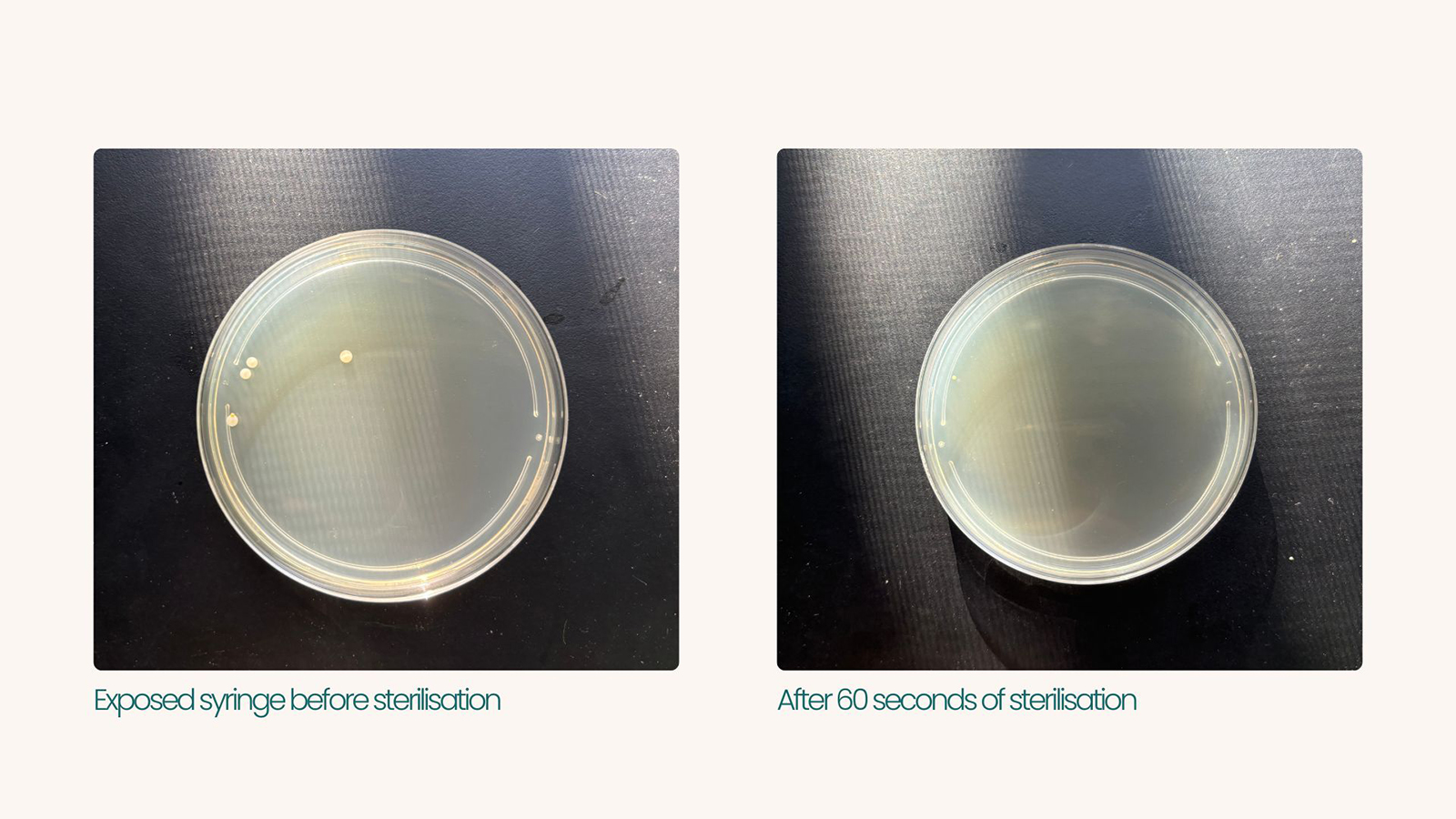
Alongside interviews, research was conducted to look at potential methods of sterilisation. The biggest challenge was overcoming the resource constraints, as the device could not rely on water, gas, or consumable supply. Ideation led to several concepts that were evaluated by the interviewees, alongside medical device design experts. Eventually, the method of using UV-C light to sterilise syringes was found to be the most viable option. UV-C sterilisation posed a few issues in efficacy due to light paths and dosage, as well as potential degradation of the syringe material. Calculations, dosage mapping, iterative design and testing revealed that the dosages received would be enough to eradicate HIV in 60 seconds. The degradation testing also revealed no signs of material failure after 12 hours of continuous dosage.
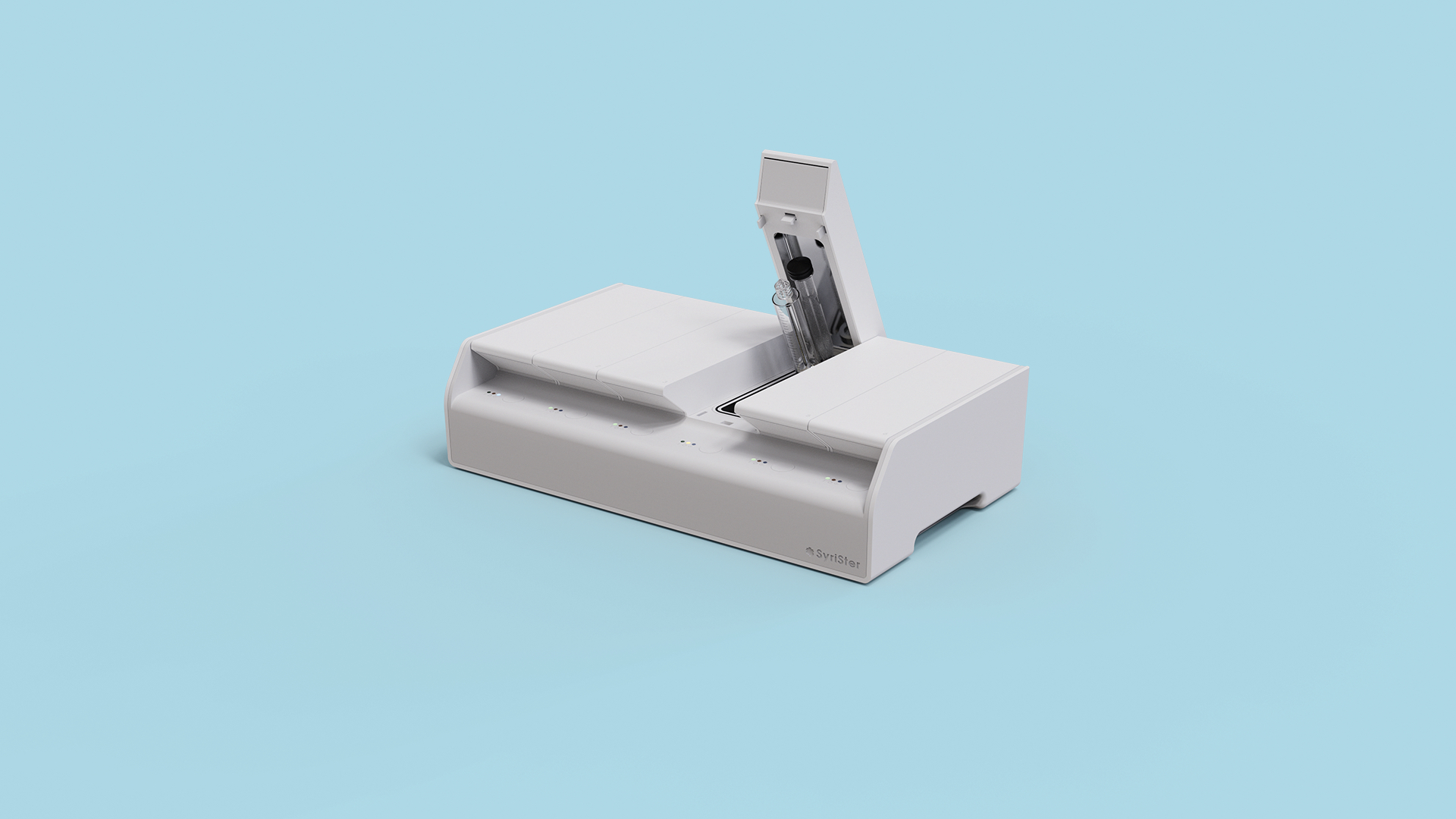
In parallel, iterative prototypes and custom PCBs were created to complement the testing, as well as narrow down robust design for manufacture and assembly. As the product would be needed for crisis zones/low socio-economic areas, low cost was essential. Work was put into making the chassis injection mouldable, as well as using LEDs to keep PCB costs down, totalling a cost per unit of $655 AUD. Usability research showed a need for storage of the syringes after sterilisation, so that users would not prematurely dispose of the syringes and be left with a short supply to resterilise. These findings led to the additions of an o-ring seal and intuitive lighting indicators to show the user the chamber status.