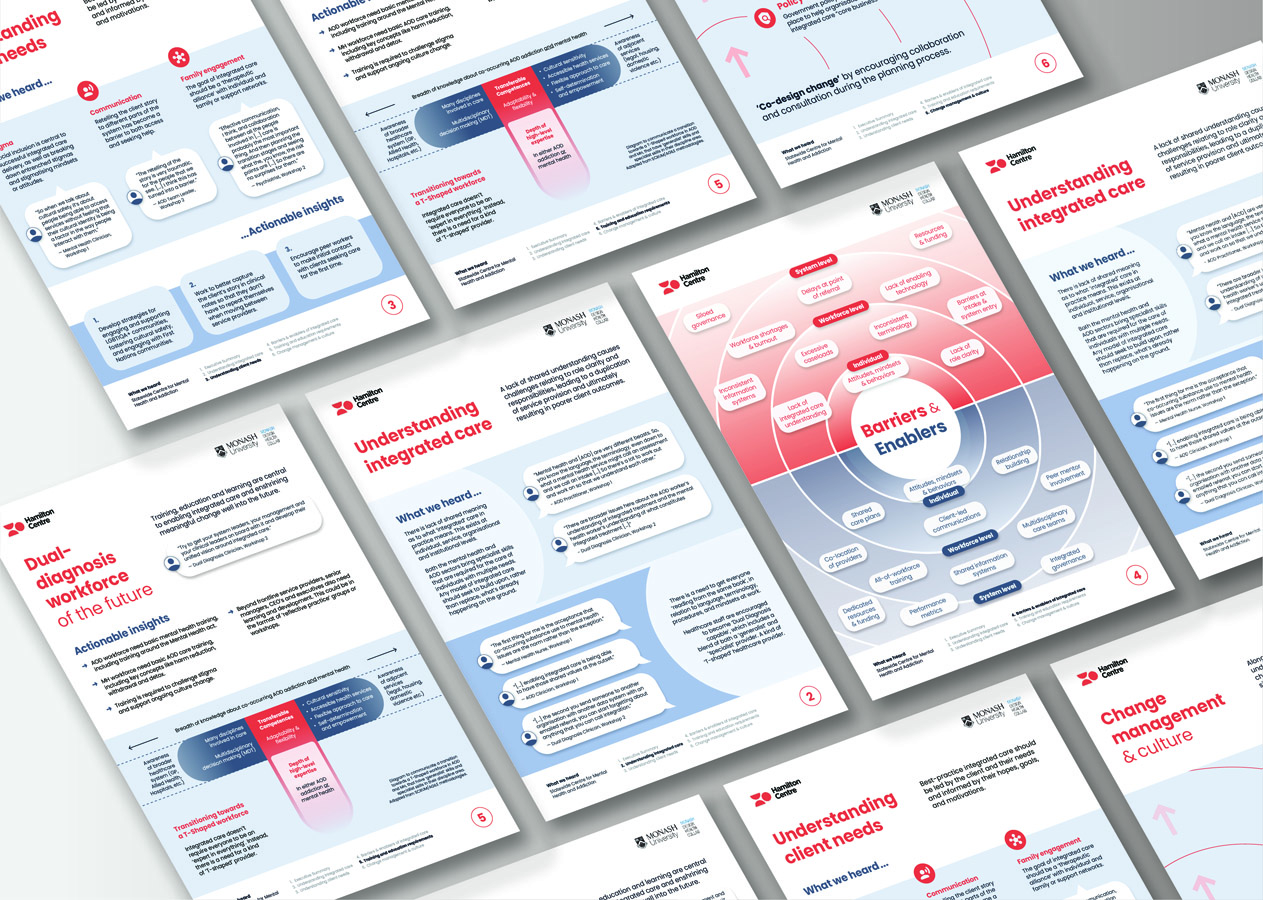
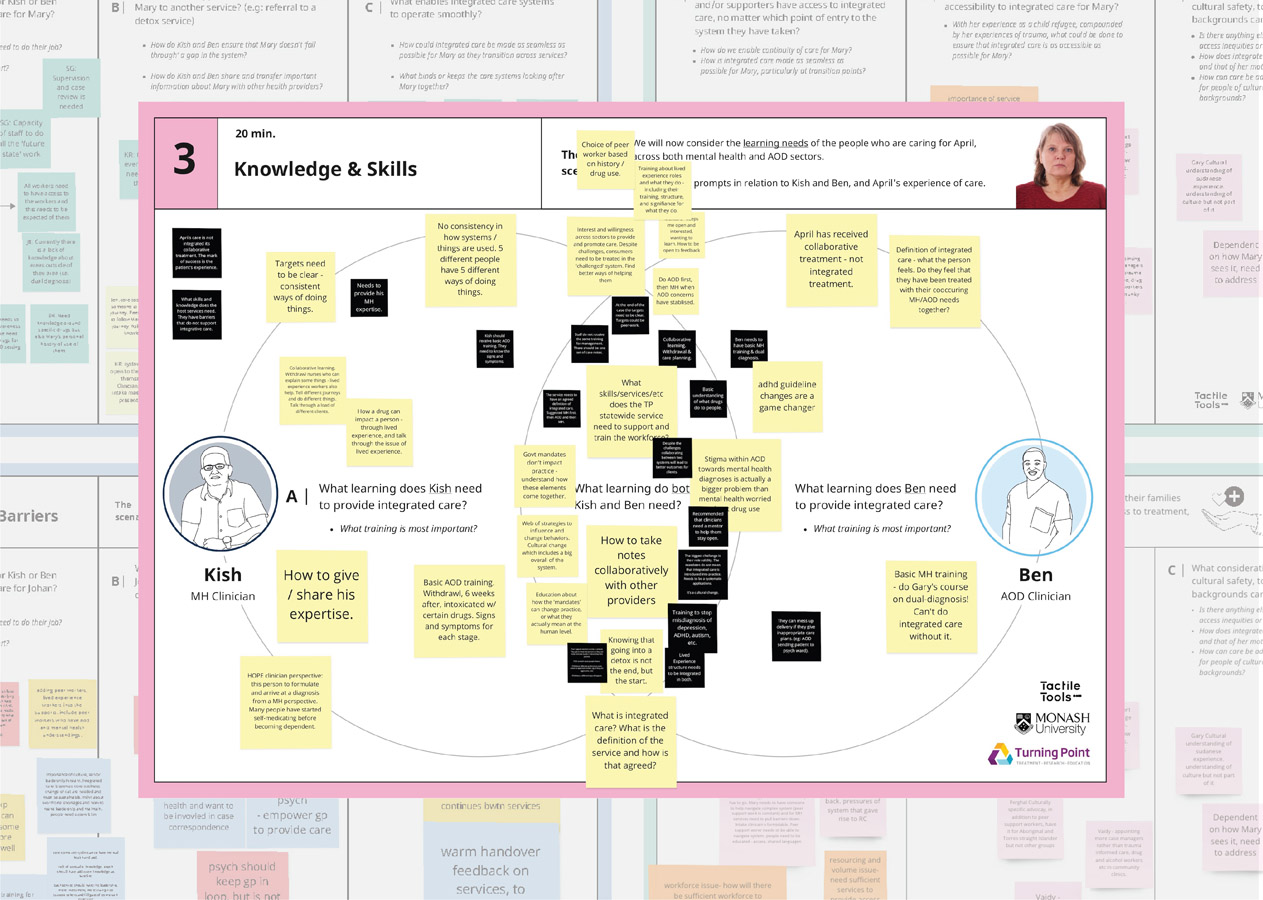
The design process for the Hamilton Centre was a comprehensive and collaborative effort aimed at creating an integrated care model that addresses the needs of individuals with co-occurring mental illness and substance use disorders. This process began with extensive co-design consultations, engaging 57 participants from over 40 organisations across Victoria, including mental health (MH) and alcohol-and-other-drugs (AOD) sectors, clinical leaders, peer workers, government officials, and lived experience advocates. This collaborative effort was structured around multiple phases, focused on identifying system-level barriers, training needs, and cultural change initiatives to develop a best practice model for integrated care that supports the new Hamilton Centre.
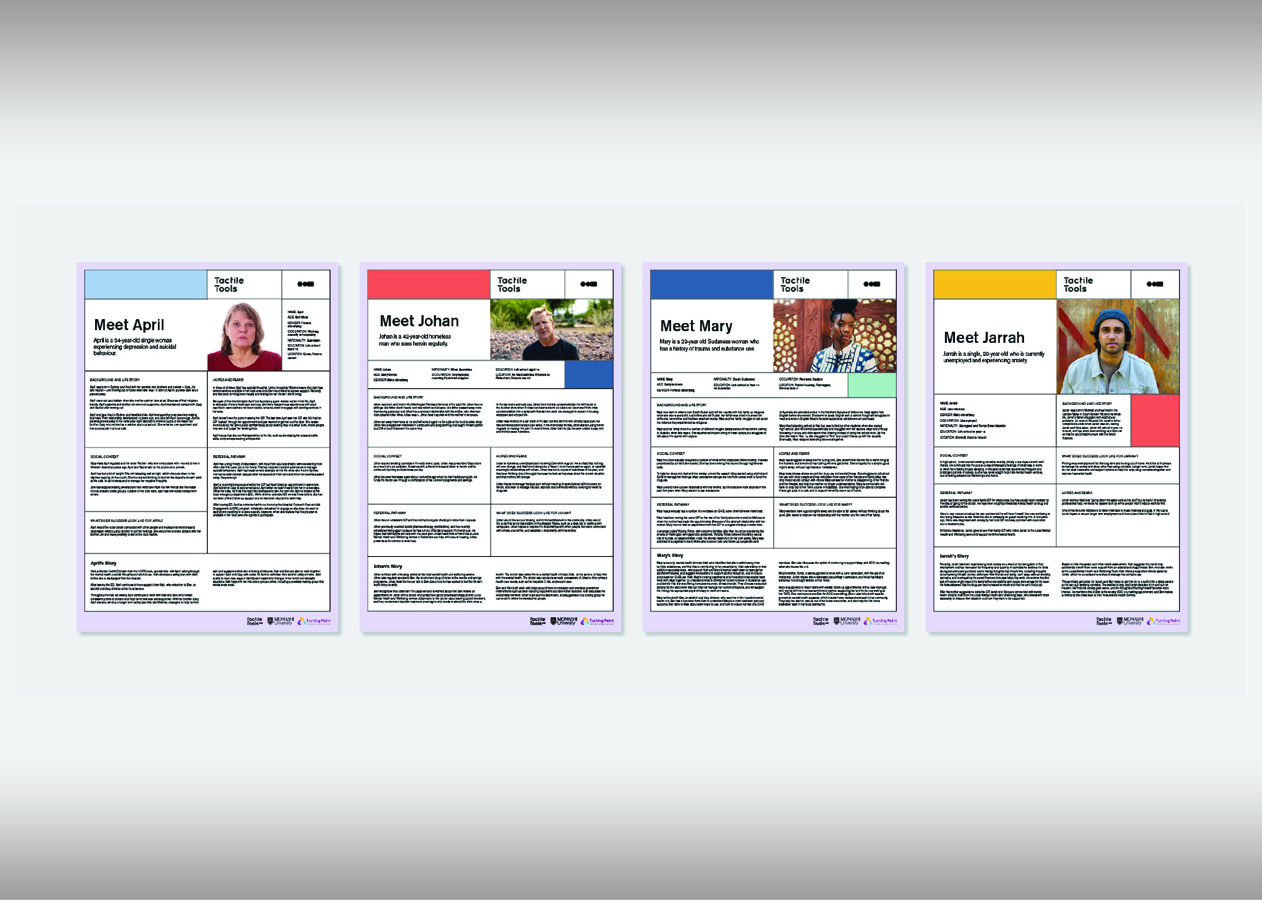
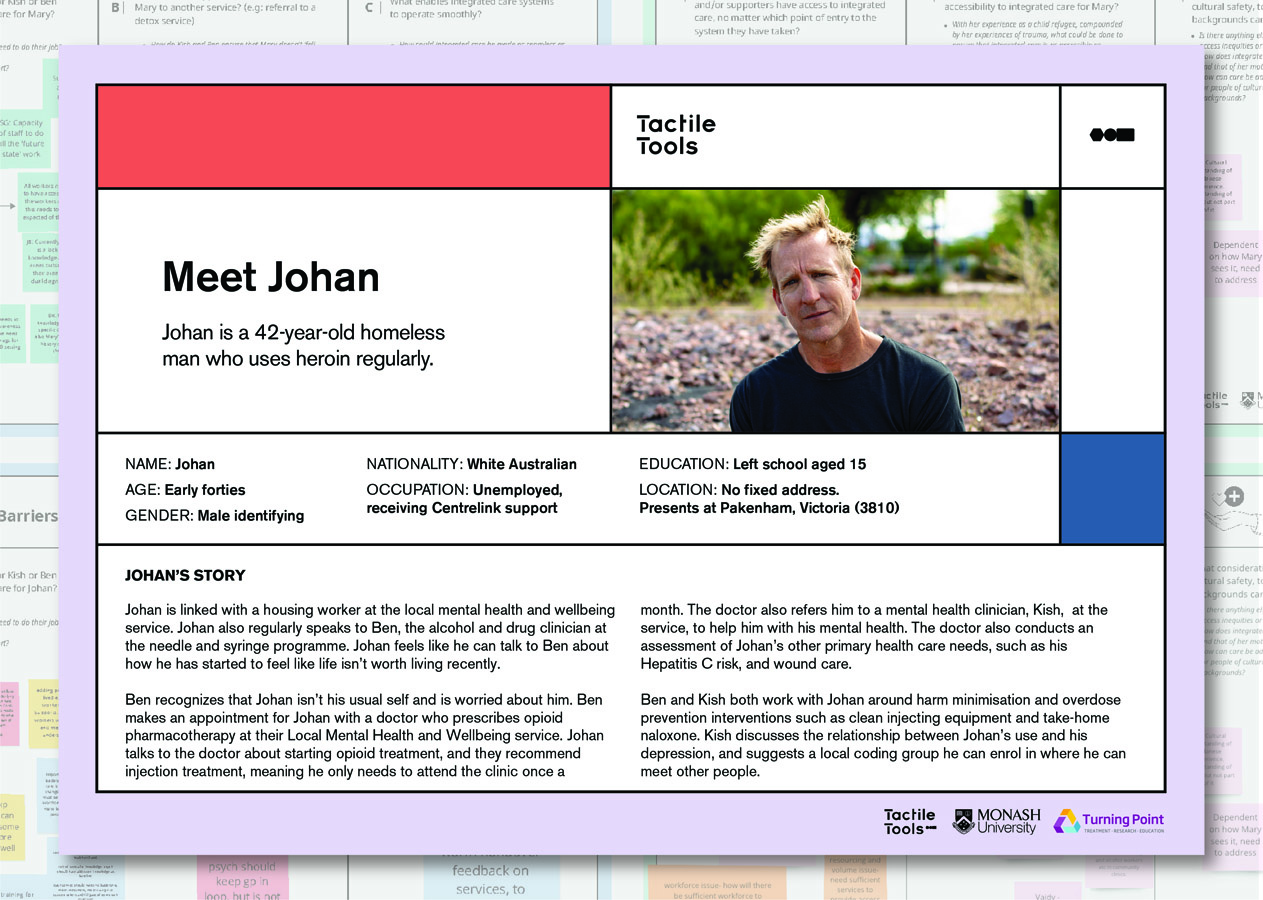
Sequenced co-design workshops were anchored through the lens of lived experience, through the development of persona narratives that sought to represent MH and AOD service users in Victoria. These personas were co-designed and iterated, in consultation with design practitioners and researchers, and then eventually with co-design workshop participants themselves. This iterative process ensured that the model developed was responsive to the needs identified by stakeholders.
By embedding lived experience at every level of development and operation, the Hamilton Centre’s design process has created a robust, responsive, and inclusive service model that addresses the complex needs of individuals with co-occurring mental health and substance use disorders. The co-design process laid the foundation for the Hamilton Centre’s governance and operational structures, where regular meetings with clinical network partner providers were established to develop the model of care, guidelines, and memorandums of understanding (MOUs) for primary and secondary consultations across the state. Regular feedback meetings with stakeholders - established through the initial co-design process - ensure ongoing refinement, adaptation and growth of the Hamilton Centre and its service model. The co-design process has also guided the development of multimodal, cross-sector education and training, and public digital information dissemination.