To address the challenges faced by healthcare providers treating compensable patients, we conducted interviews with a diverse range of medical practitioners from various disciplines, including General Practitioners (GPs), Physiotherapists, and Psychologists, from all around Australia. This group also had varying opinions and experiences working with and treating compensable patients from schemes such as WorkCover and TAC.
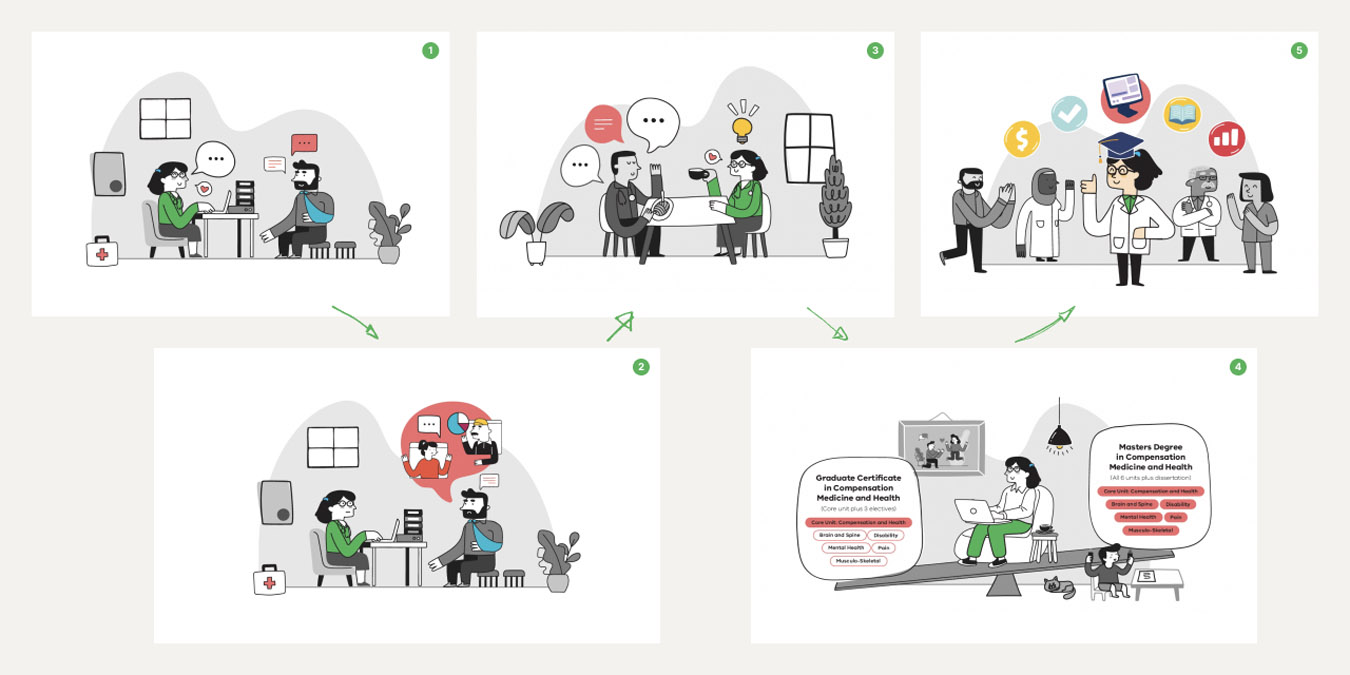
We used semi-structured interviews and storyboards as a way to test the hypothesis of a post-graduate Masters program would be valuable. These insights were used to refine the Masters program’s value proposition, ensuring it meets their needs more effectively. We also explored and tested new ways to improve access to compensable medical knowledge and professional development.
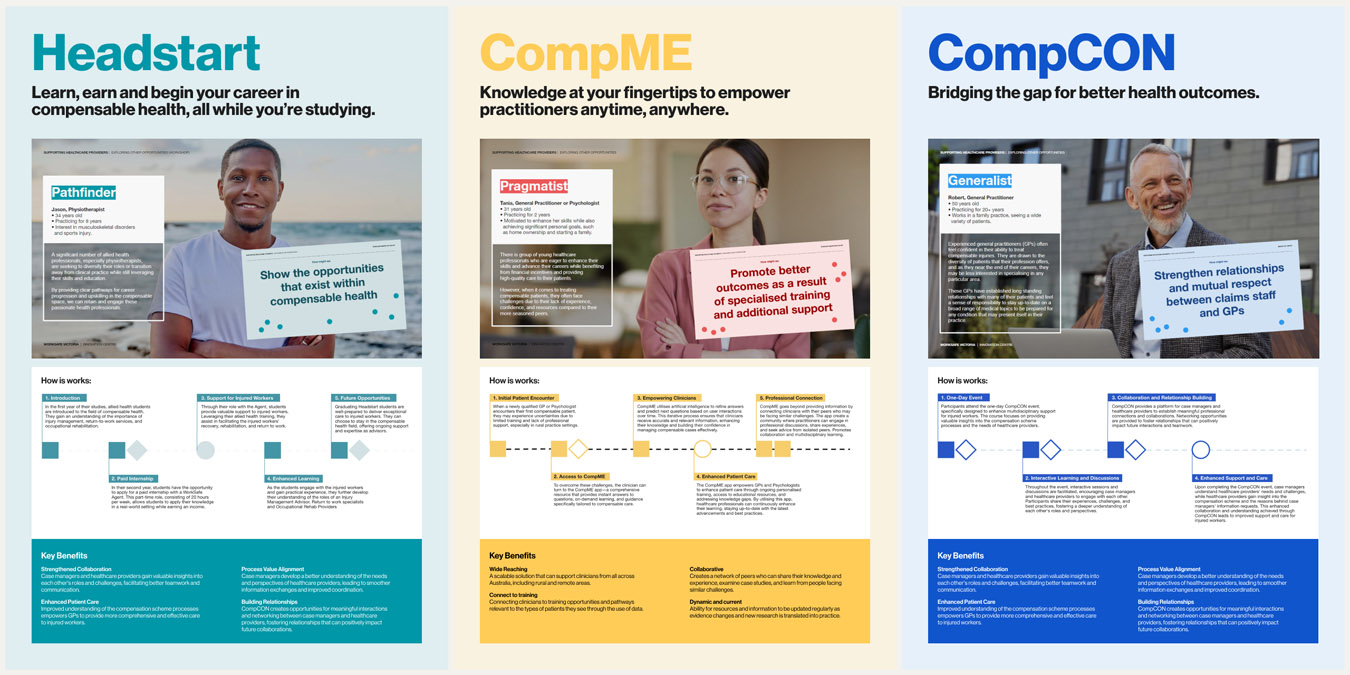
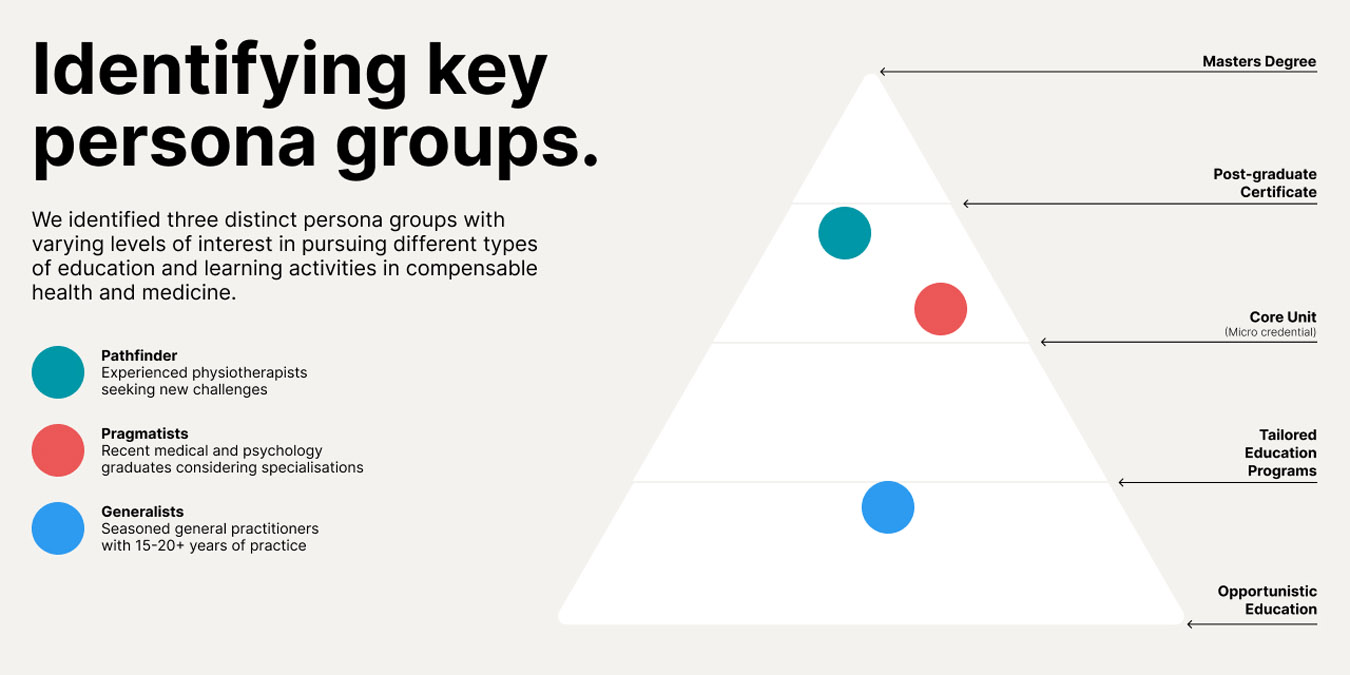
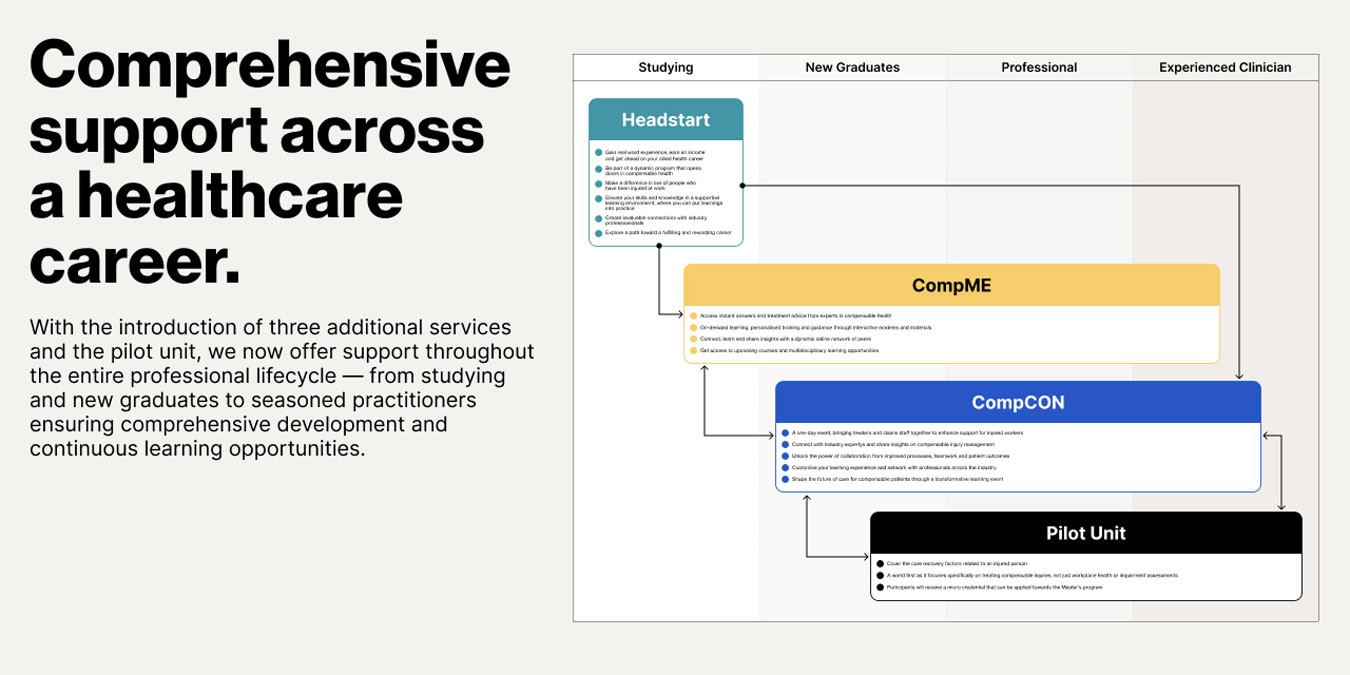
To further understand these opportunities, we developed personas representing the different healthcare providers who were interested in elevating their compensable knowledge. These personas helped us frame ”how might we” questions, which were tested during a co-design workshop with a group of practitioners and representatives from WorkSafe, TAC, Comcare, PIEF and health providers working in advisory roles. From this workshop, the ideas and concepts were refined into three additional services:
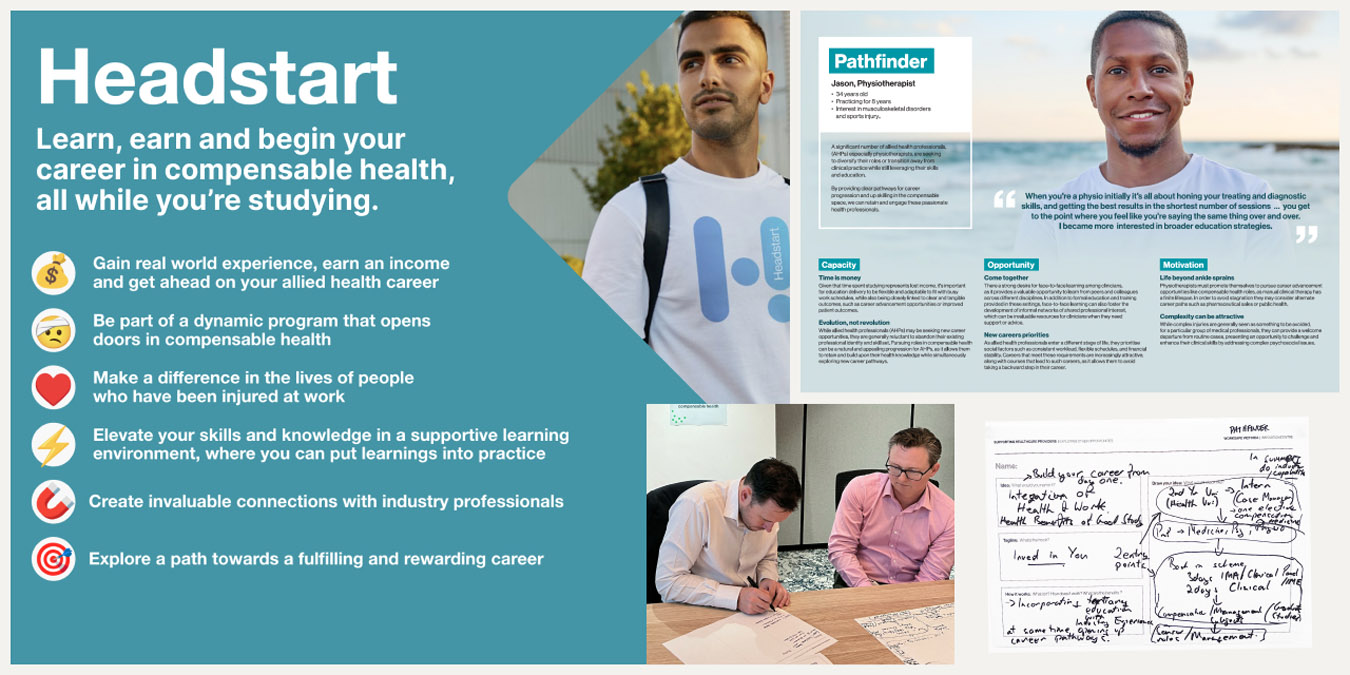
- Headstart: A paid internship program for allied health students to gain hands on experience in compensable health practices
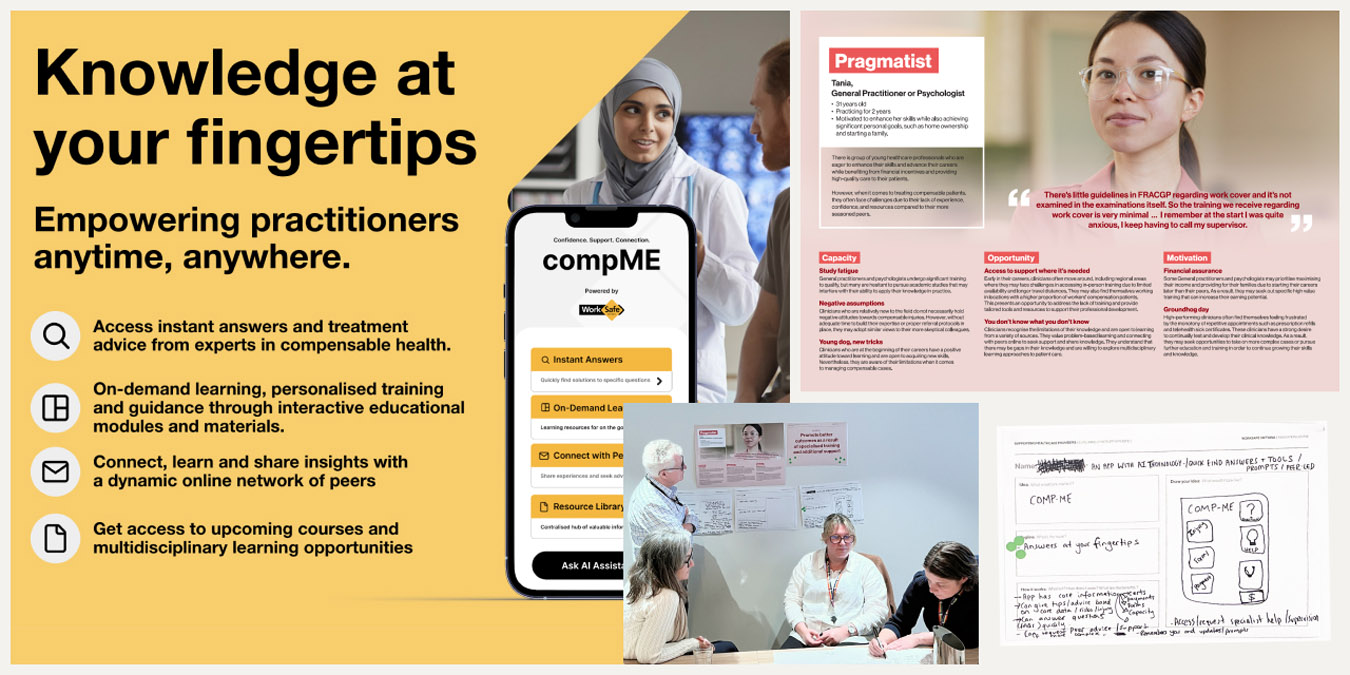
- CompMe: An app designed to support rural practitioners who often have less access to support and resources to treat compensable patients confidently
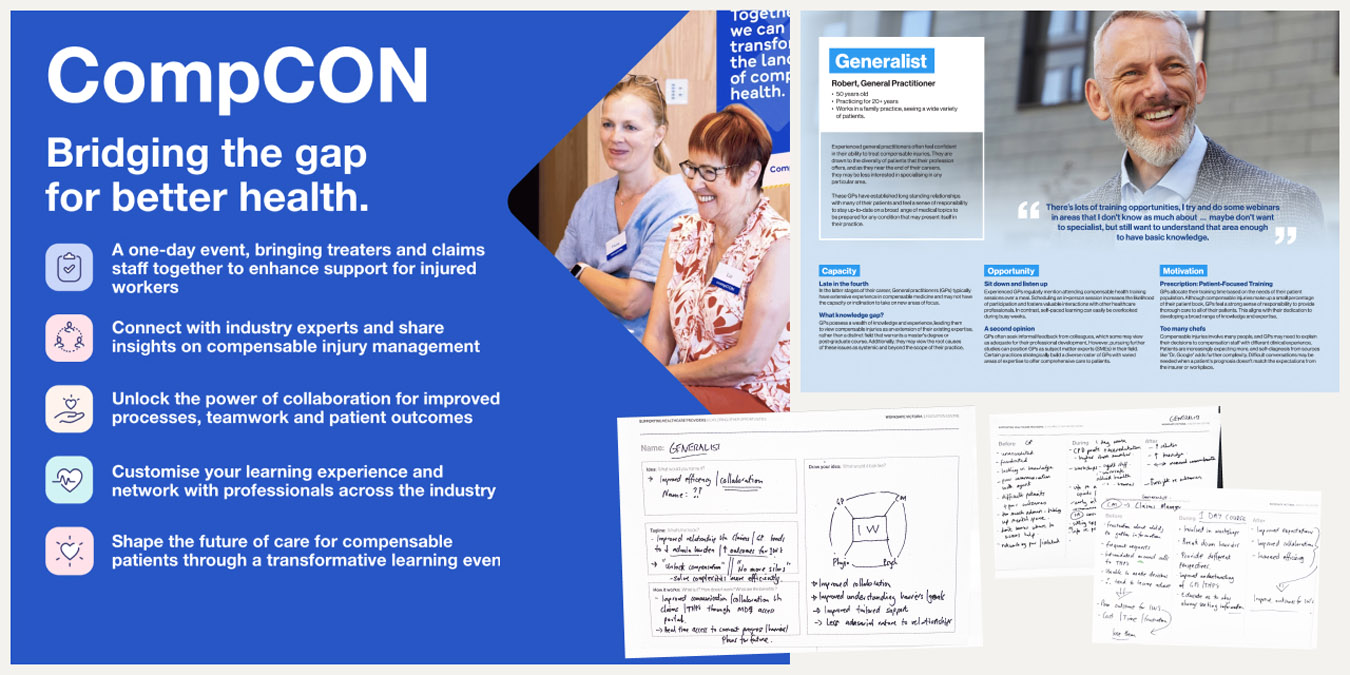
- CompCON: A conference for case managers and healthcare providers to collaborate on compensable health to foster better relationships
Our recommendation for the Masters program pilot was endorsed by PIEF. Monash University is developing this unit, scheduled to launch in 2025.