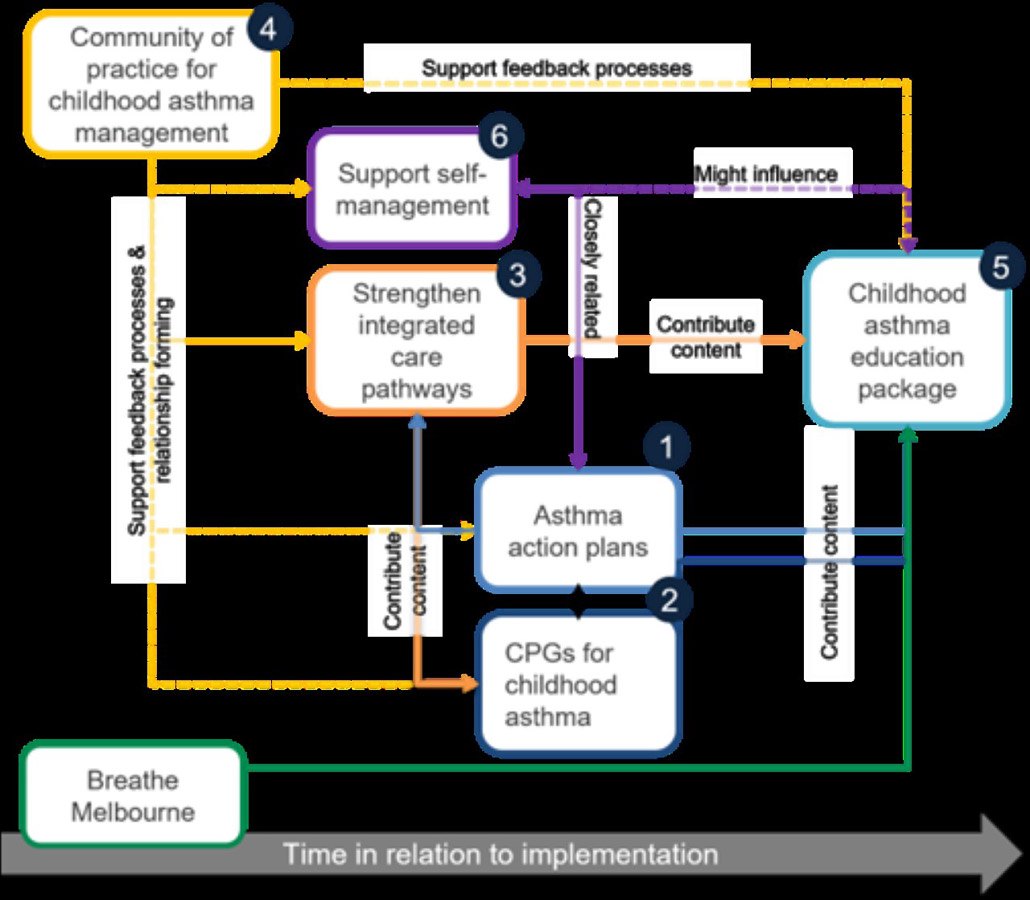
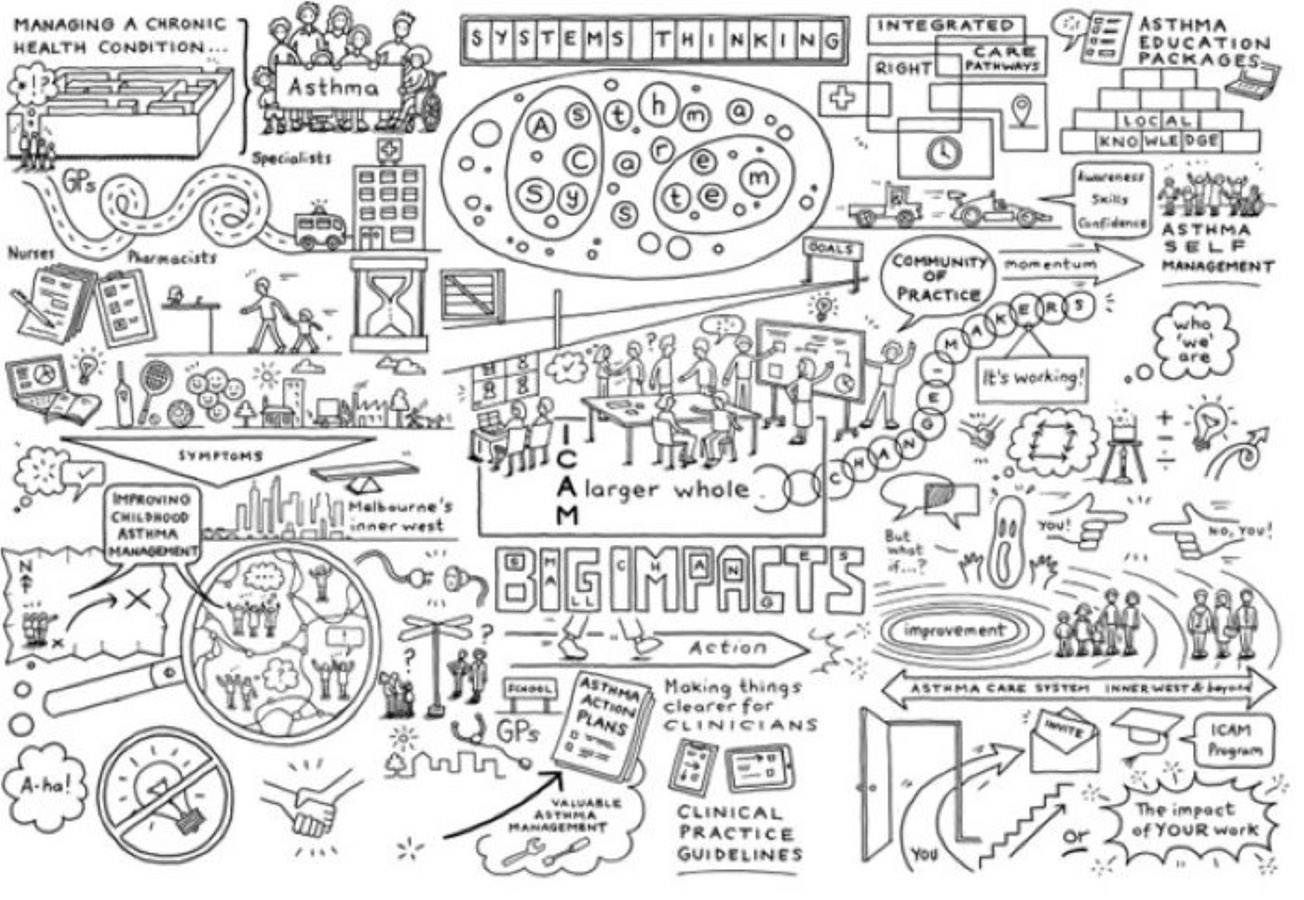
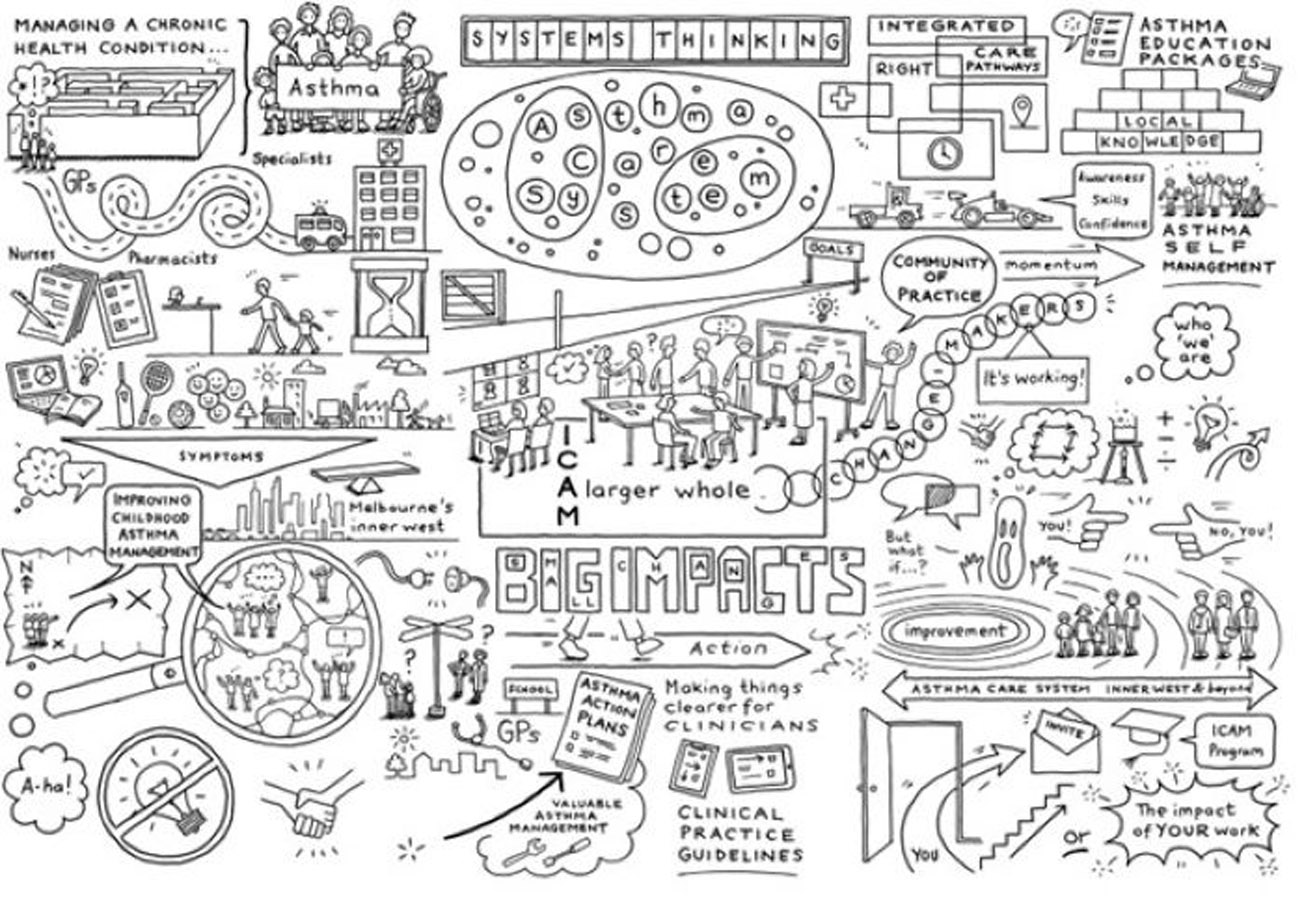
A system thinking specialist was engaged to assist and map the relationships, flows and dynamics between many separate agents involved. This involved engagement with over 25 different organisations and consumers to unearth the multiple perspectives and forces underpinning the behaviours seen. The resulting system map generated new perspectives and understandings between each component and was the basis to locate areas for intervention.
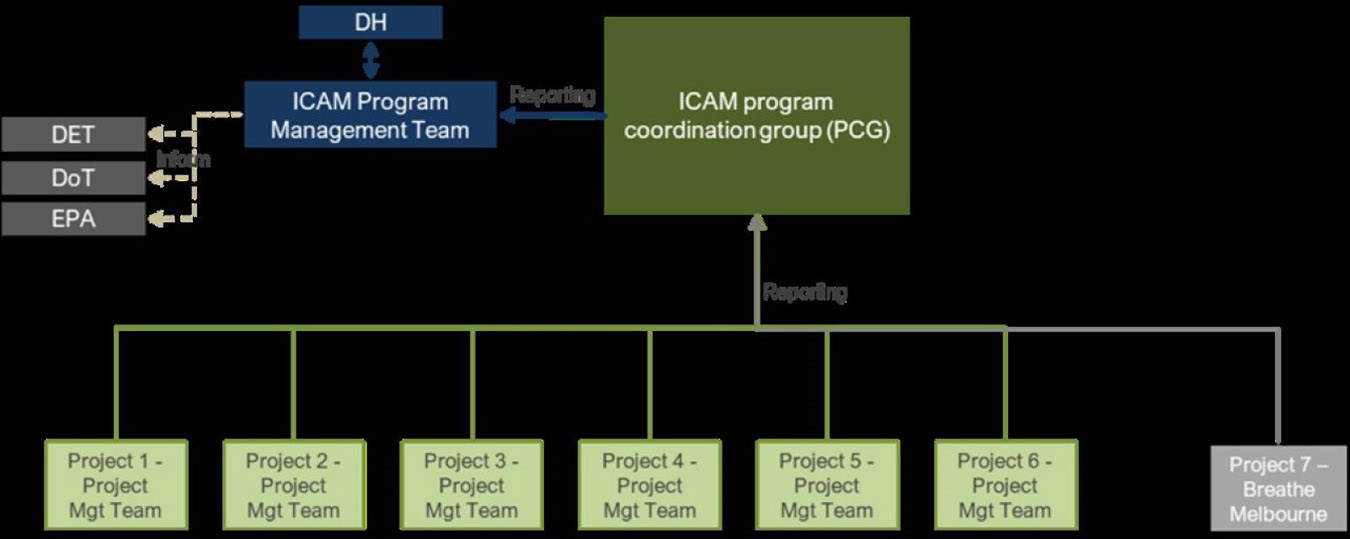
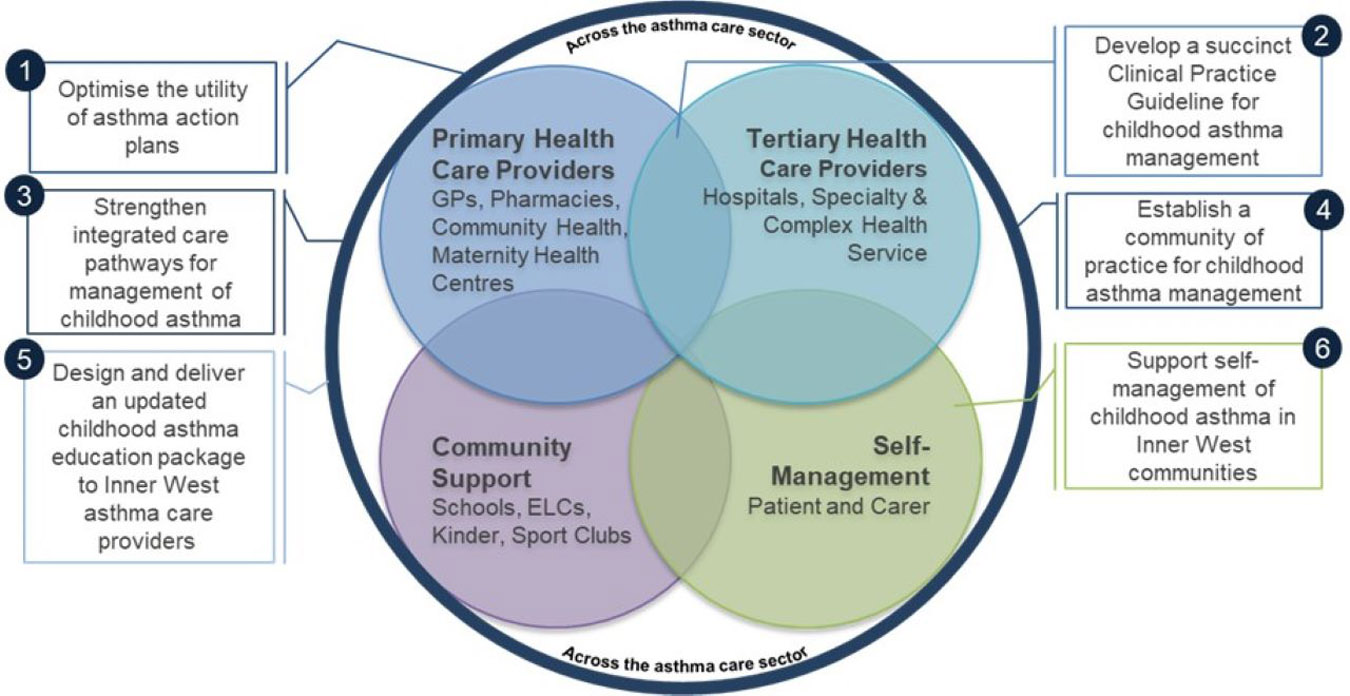
The DH ICAM team oversaw the program comprised of six interlinked projects, and adopted a unique approach, allocating projects to the following organisations:
- Asthma Australia (AA)
- National Asthma Council of Australia (NACA)
- cohealth
- Royal Children’s Hospital (RCH)
- SCV
SCV in partnership with North West Melbourne Primary Health Network lead the Community of Practice (COP) involving cross-sector and interdisciplinary clinicians, and representatives from government, peak bodies and consumers. The CoP convened virtually each month, and was co-facilitated by a by a paediatrician and a local General Practitioner to emphasise the importance of integrated care. This forum not only provided information about asthma care and services but was a safe space to generate and galvanise relationships, raise issues and work together towards possible solutions, given that relevant local stakeholders were in attendance to make improvements.
SCV utilised the Model for Improvement to design the strengthening integrated care pathways project. Seven sites participated, including general practices, community pharmacies, and hospitals. The pilot consisted of five virtual workshops and one-to-one coaching with an improvement coach to build improvement science capability, promote cross-sector collaboration and empower clinicians to make changes to their local health services.
Achievements:
- Twenty-nine change ideas were identified, tested, and implemented across sites. *Case studies demonstrated service improvement
- Increased referrals to the cohealth community asthma program
- CoP and the integrated pathway project extended to the north and west region of metropolitan Melbourne in a new phase