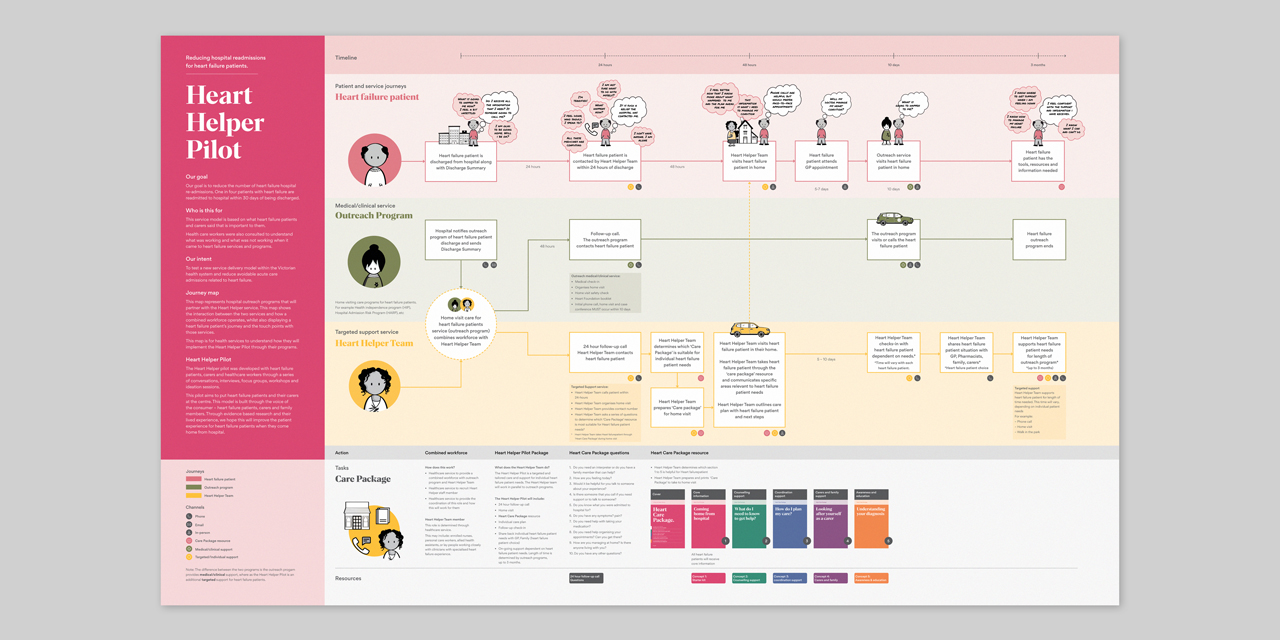
The project approach was crafted to respond to the unique needs of the public sector and is based on the Victorian Government’s Human-centred Design playbook and Safer Care Victoria’s Partnering in Healthcare Framework. The design process placed the healthcare system stakeholders at the centre in a process that brought together aspects from both human-centred and co-design approaches. The design process responded to the complexities of Victoria’s healthcare system by employing a range of design methods to comprehensively engage with all stakeholders in the system, including lived experience consumers, heart failure patients, carers, family members, clinicians and healthcare workers.
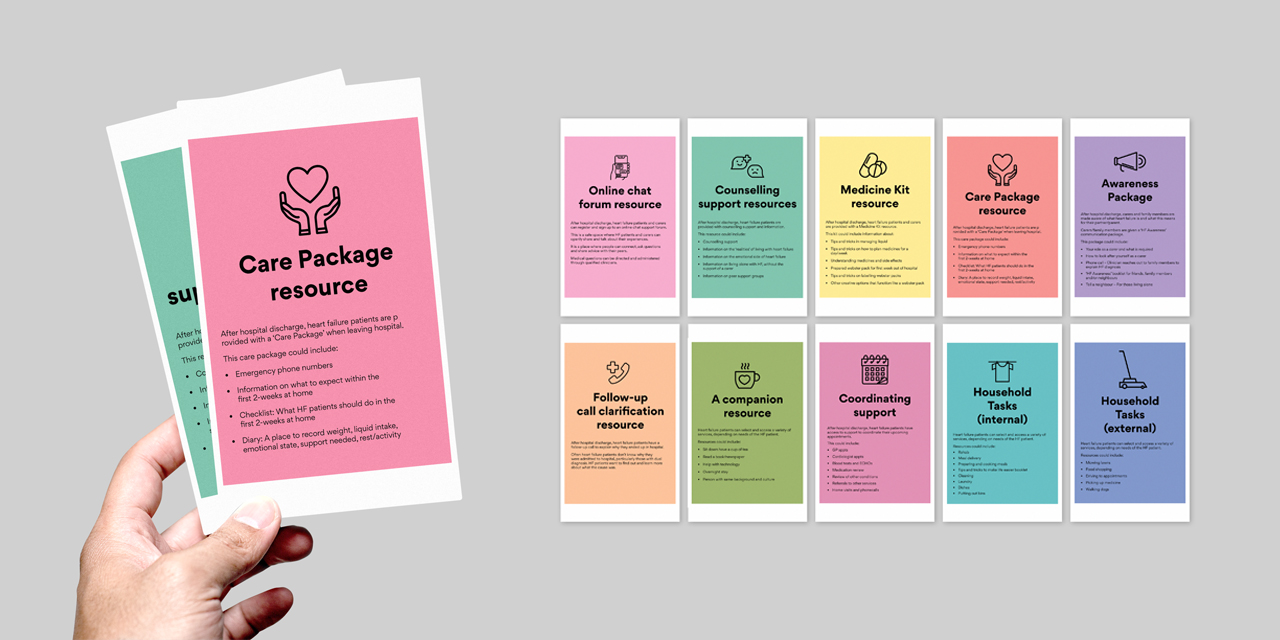
This ensured that the outputs designed had considered the needs and experiences of the patients within the current assets, challenges and realities of the hospital system and health service delivery for those needing heart failure care. We did this by involving system actors throughout the design process:
- Listening to and observing patients: 1-1 interviews with heart failure patients with different lived experiences (e.g. Newly diagnosed, multiple diagnoses, with and without external support); Observation study with patients enrolled in at-home care.
- Hearing from carers and family members: 1-1 interviews.
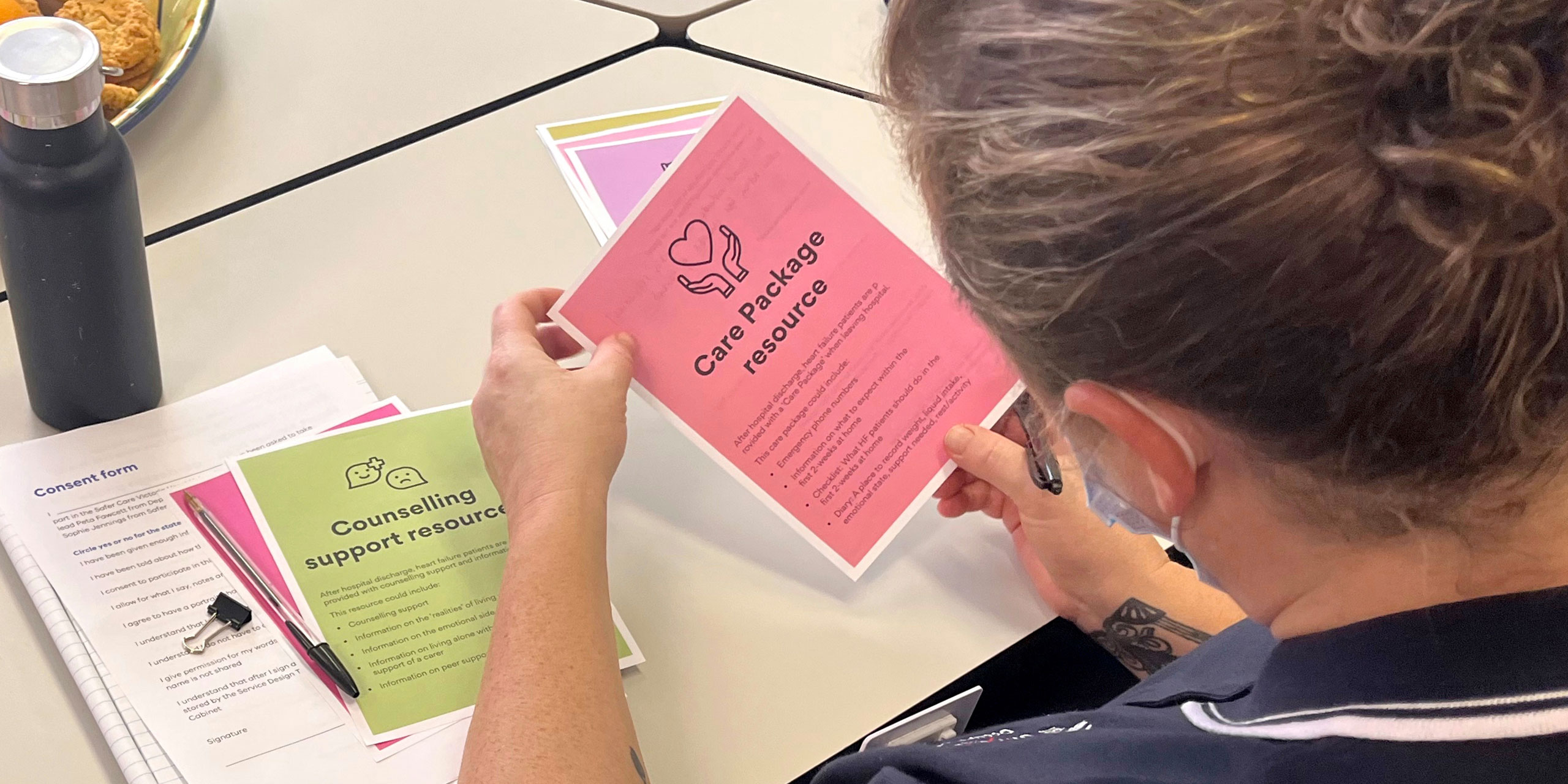
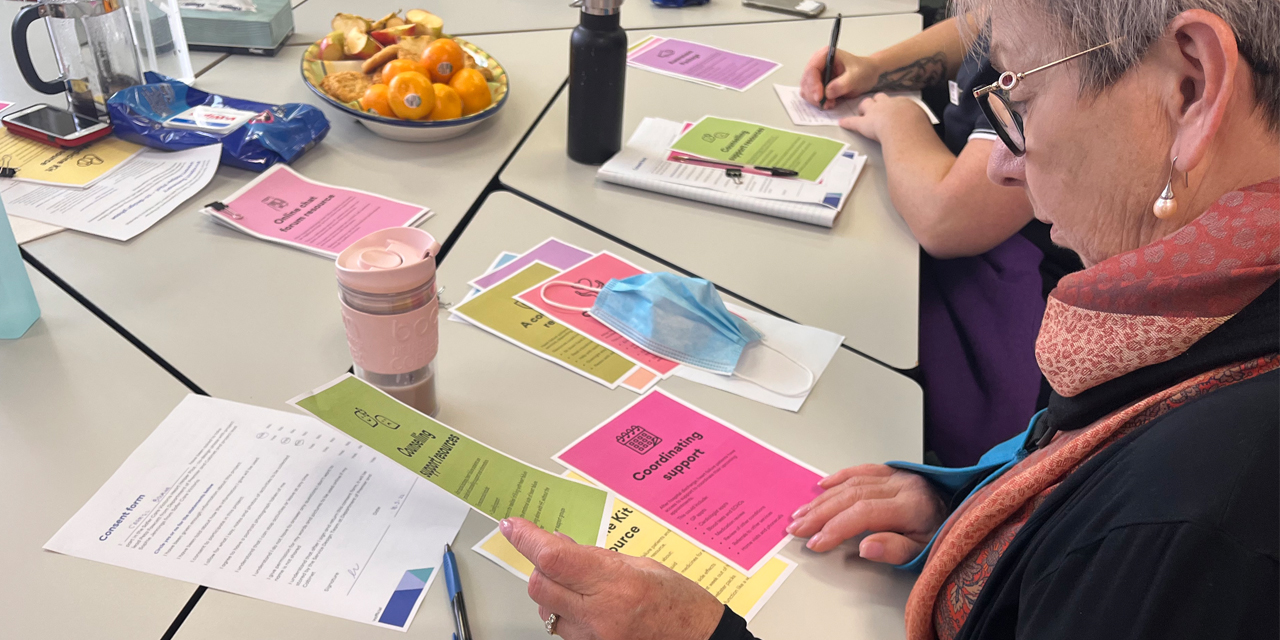
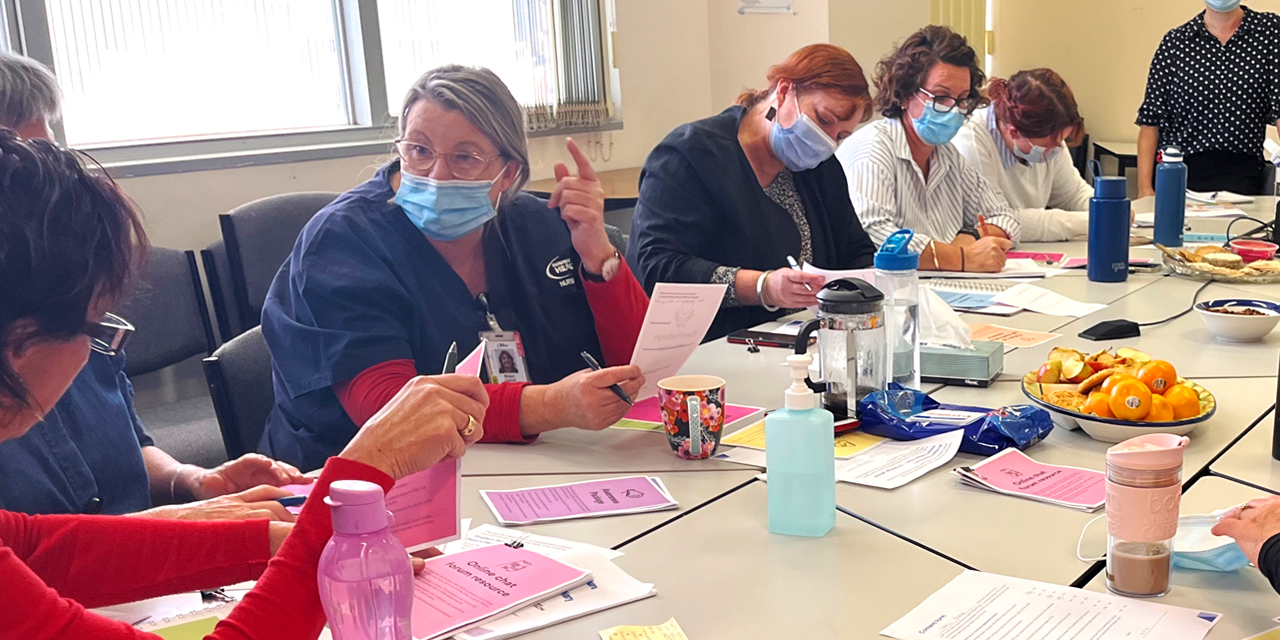
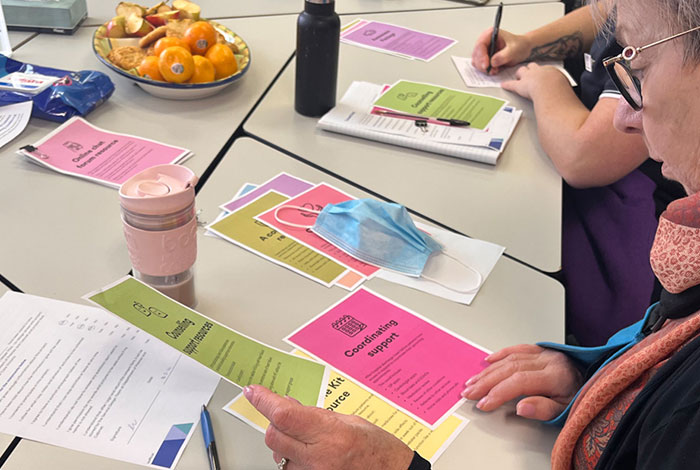
- Shadowing and prototyping with healthcare workers: Focus groups with staff from healthcare services in regional and metropolitan Victoria; Shadowing healthcare workers in hospital; Prototyping sessions to develop and test concepts with healthcare workers.
- Employing a lived experience consumer as a design team member