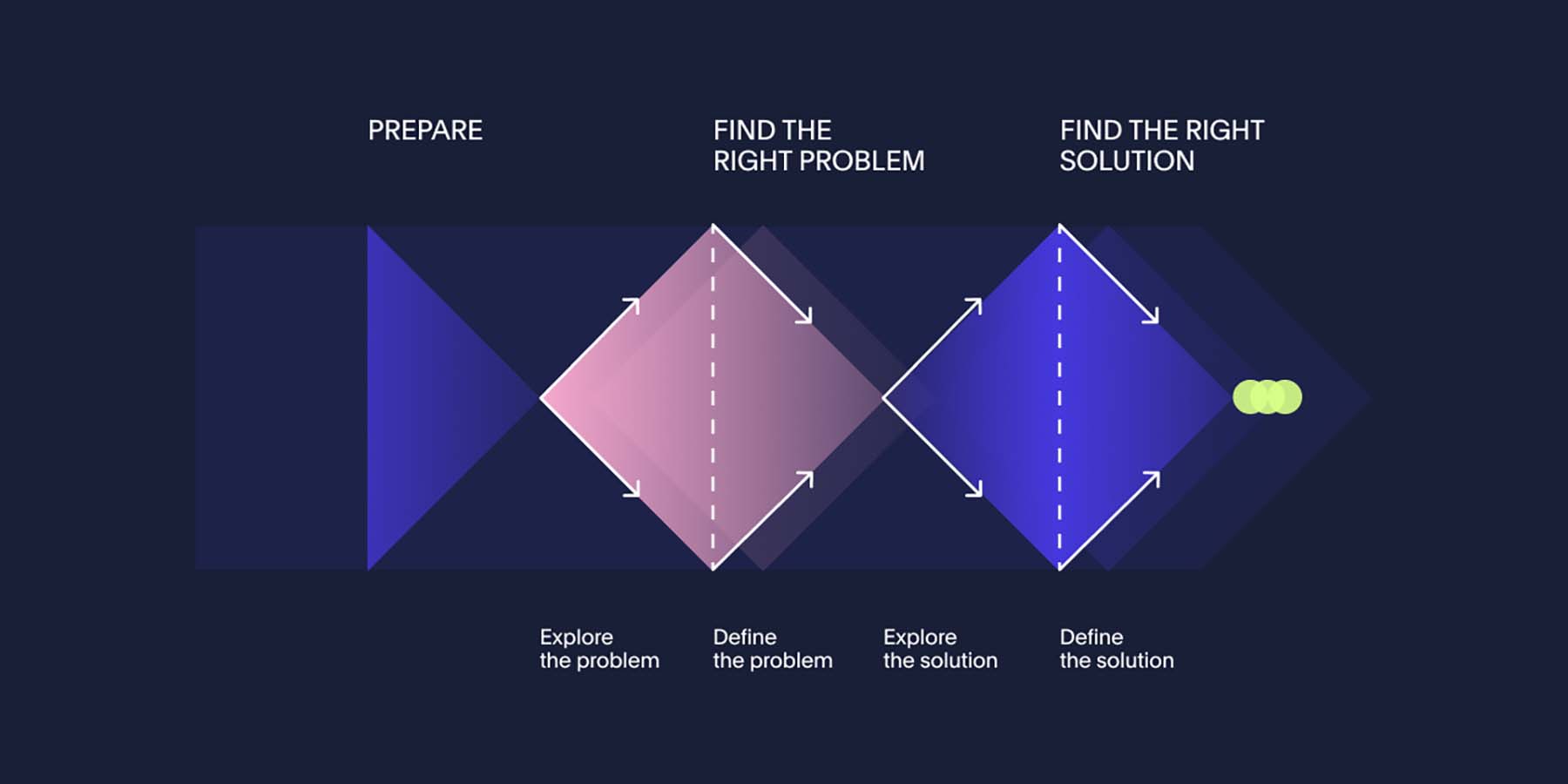
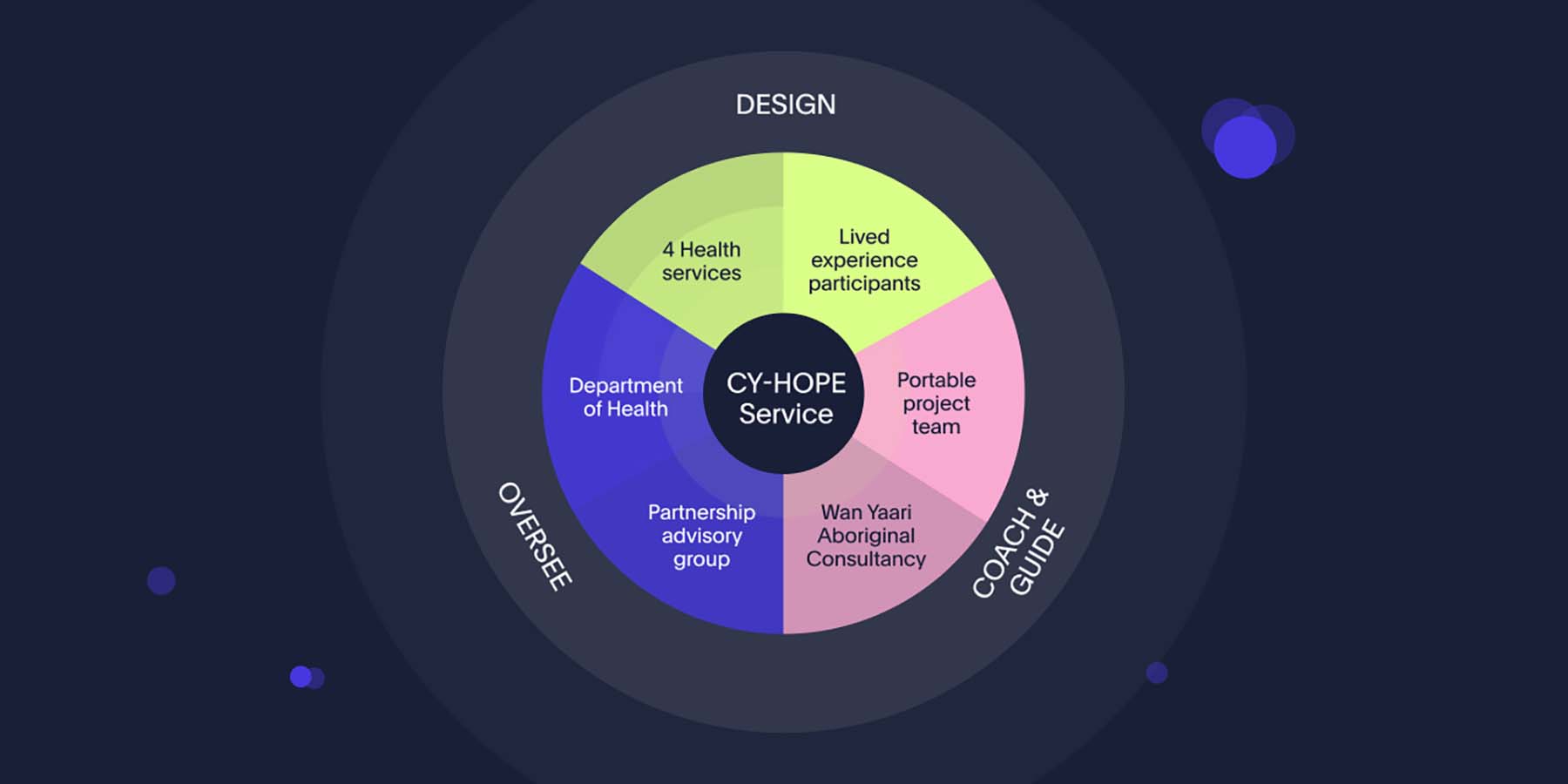
Beginning with a 2-day co-design training course, we introduced the Department of Health and the health services to key concepts with a practical application of design activities. The training also included mindsets for social co-design, Portable’s mental health design principles and ethical considerations for power-sharing and participant safety. We then individually coached the health service design teams through each stage of the co-design process, to support them in designing the service with people that have lived experience. Coaching at each stage included:
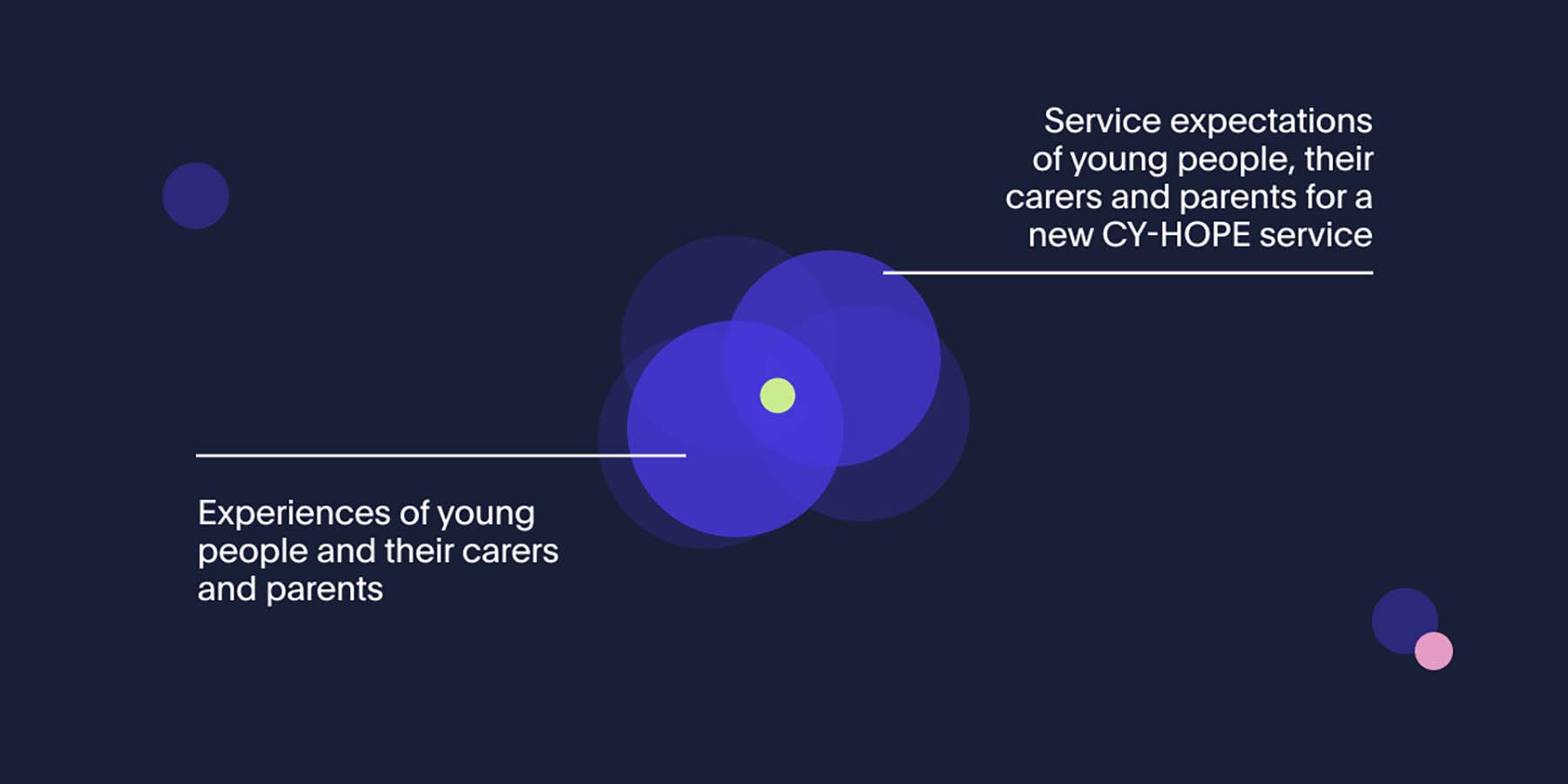
Exploring the problem: Health services immersed themselves in the experiences of those they are designing the Child and Youth HOPE service with. They used a range of methods and activities to gain a deep understanding of those with lived experience and those who provide professional support, including workshops, contextual interviews and emergency department data analysis.
Defining the problem: Health services organised all their findings and grouped them together in related themes and ideas. Then they started to build a picture of the current end-to-end journey people go through and what they need at each stage in order to feel supported.
Exploring the solution: We encouraged lived experience participants, lived experience leads and health service staff to be as imaginative and unrestricted as possible in their thinking at this stage, so that they could explore many possible ideas for solving the problem. Potential ideas for the new Child and Youth HOPE service were distilled into a concise and formulated concept, visualised as a prototype.
Making the solution work: As teams moved through the co-design process they identified constraints, assessed and prioritised their ideas to refine the prototype that would balance what was desirable, viable and feasible. Health services tested and iterated their prototype until it was developed enough to inform a final Child and Youth HOPE Model of Care.